How to Tell If Diet Mismatches Genetic Determined Metabolic Ability
A few practical tips on doing this modified fasting diet are in order. Timing
this around what is going on in life can be helpful. It gets harder during stressful times. This made me appreciate how “stress eating”
is a problem in the first place. In
contrast, this gets easier during times of high constructive activity. It seems if we are meaningfully engaged, we
don’t get as preoccupied with eating.
The moral is that controlling stress and being busy with meaningful
activity is a poorly appreciated part of good dietary behavior.
On to the issues of what is happening with our eating
behavior and why a modified fasting diet can be so helpful. The real issue with the current Western diet
for the majority of the U.S. population is that its composition places maximum
stress on the portion of our metabolic machinery that is least adept at
handling it. Maximum stress on a weak
area typically will cause failure, which in this case, is chronic metabolic
disease.
That weak area is the broad group of enzymes used to
manage a main end product of carbohydrate digestion - sugars. There are many dozens of different enzymes
involved in the process of trying to convert sugars into energy. As we previously discussed, when the amounts
of sugars exceed the need at the moment, it goes to the liver to be converted
to the fat, triglyceride. The
triglycerides are then circulated destined for fat storage in the central
(abdomen) portion of the body. If
carbohydrate/sugar intake chronically exceeds the need of the moment,
triglyceride is increasingly produced and fat stores increase.
One of the primary features of the Paleo period genetic
pattern is multiple SNPs of the genes involved in processing sugars to
energy. The 75-80% of westerners who
have this pattern just cannot manage high amounts of carbohydrate/sugar under
normal circumstances.
A great question to answer might be how much
carbohydrate/sugar does one consume?
By all measures the amount of carbohydrate in the western
diet has increased from 200-600%, yet the genetic ability to manage it has
literally not changed. The second and
equally troublesome factor is the “glycemic load” of the western diet. Glycemic load is a combination of how much
and how fast a given carbohydrate will raise blood sugar. Not all carbs are created equal. Simple sugars and grains have a
disproportionately high glycemic load compared to fruits and vegetables. Simply put, they generate far more stress per
gram on metabolism than other carb sources.
A great analogy might be a worker who can process 50
files very accurately in a 40-hour work week.
If you want to make this good worker make a lot of mistakes you can do
it one or both of two ways. Have them try to process 200 files in the same week
(increased amount of carbohydrate), or have them try to process the same 50
files but only working 2 hours a day for the 5 days (high glycemic load). The western diet is like having that worker
try to do both!
So how do we tell if we are in metabolic stress trying to
manage carbohydrates? The first sign is
white adipose tissue or belly fat which is stored triglyceride.
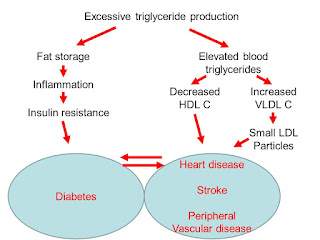
Additionally, when liver triglyceride production is high, the production of HDL or “good cholesterol”
drops and the production of a very small cholesterol molecule, VLDL,
increases. These VLDL particles are particularly
worrisome as they become very small dense LDL which is the most dangerous
regarding vascular disease risk.
The last step in this metabolic dysfunction cascade is
that the insulin resistance so impairs the ability of cells to take in sugars
to burn or convert to triglyceride that blood sugar rises. At the first sign of this the diagnosis of
“pre-diabetes” is made, and as it progresses it is eventually called
diabetes. Pre-diabetes is like calling
the first trimester of pregnancy “pre-pregnancy”. I think it should more appropriately be called
simply early diabetes.
That was a lot so I’ll summarize. The common order of problems showing up
suggesting metabolic distress in handling carbohydrates is:
1) Belly
fat – excess triglyceride
2) Increasing
blood triglyceride - >125 mild concern, >150 real concern
3) Decreased
HDL - < 40-50. A triglyceride/HDL >3 is a real concern
4) VLDL
cholesterol >30
5) Increased
small LDL particles – requires specialized testing called an NMR profile
6) Increased
blood sugar
The small LDL particle size needs a little
explanation. We generally make two sizes
of LDL or “bad cholesterol”. The size of
the particles determines their ability to cause vascular disease with small,
dense particles being more dangerous than large, fluffy ones. We all make some of each but in varying
ratios. Genetics influence this ratio
some, but diet also highly affects it.
While person “S” and person “L” have the same total
weight of LDL, person “S” on the left side has many more small particles and
therefore greater risk.
Some persons with “normal” LDL cholesterol levels develop
vascular disease while others with relatively high LDL cholesterol never
will. The particle size and number
variable is thought to be an important determinant of this contradictory risk.
The point of all of this is that before blood sugar
inches up into abnormal range, the body has been firing warning shots across
the bow for many years with the above changes in body and blood profile. Diabetes is a late effect of chronic
metabolic chaos.
A minority in western populations can tolerate a greater
percentage of carbohydrate and a somewhat higher glycemic load. This is like the uncle someone has who smoked
a pack of cigarettes and drank a quart of whiskey each day living to be
relatively healthy until killed in a skydiving accident on his 90th
birthday. We all assume we are “that
guy”, but they are very rare. Most of us
will need to give careful attention to matching our diet chemistry to our true
metabolic ability. Not doing so has led
to the epidemic of metabolic disease which we are trying to beat down with
drugs. The food got us there, and it is
the foundation for an effective solution.
So I continue with the modified, intermittent fasting to
help reset my metabolism. Starting with a
normal body fat I still lost 7 lbs the first 2 weeks and 1 inch off my
waist. If you take the list of the
problems that show up early indicating some metabolic stress, the modified,
intermittent fasting does a “system restore” on it all. The first indicator that that is happening is
pulling triglycerides out of belly fat to burn for energy. I choose not to curse my genetics but rather
cheer the knowledge of a solution.